Ultralow-field MRI machine could cost less than a car
DOI: 10.1063/pt.vrev.smhj
Many improvements in health care are the result of MRI. Doctors use the noninvasive imaging technique to diagnose strokes, brain injuries, tumors, and other conditions of the brain and spinal cord. The technique can image many other internal organs, and doctors often prefer it to other imaging techniques, such as CT scanning and positron emission tomography, because of MRI’s lack of ionizing radiation.
Yet despite a half century of advances since the invention of MRI, the technology is still hard to access in low- and middle-income countries. The US has roughly 40 scanners per million people, but the average across all African countries is only about 0.7 scanners per million people. 1 A typical 1.5- or 3-tesla instrument uses a heavy superconducting magnet, which must be kept cool with expensive liquid helium, and power-hungry imaging electronics. In addition, the room housing the machine must be built with extensive shielding to block electromagnetic interference.
To lower the cost and power demand, MRI researchers have been developing alternative instruments that use simple permanent magnets and thus apply a relatively weak magnetic field. But the weaker fields lead to blurry images, which obscure the anatomical detail that doctors need when diagnosing and treating various diseases.
A research team led by Ed X. Wu of the University of Hong Kong has now constructed an MRI device that produces relatively high-quality images with a 0.05 T field, 1/60th that of a conventional instrument. The new machine uses the same amount of electricity as a hair dryer, and unlike previous low-field scanners, it’s capable of imaging not just the brain but also other major organs. The researchers developed an artificial intelligence (AI) algorithm to sharpen the initially blurry images. Although the approach needs more clinical evaluation, the preliminary results show much of the same anatomical detail as images from a high-field instrument. 2
Magnetic resonance
MRI scanners work according to the principle of nuclear magnetic resonance. Hydrogen nuclei in the human body, primarily in fat cells and water, become spin-polarized in the scanner’s strong magnetic field, and in bulk the nuclei develop a small magnetization that’s aligned with the field. Then a perturbing RF pulse pushes the bulk magnetization out of alignment so that it precesses about the applied magnetic field, similar to how Earth’s rotational axis wobbles slowly over time.
The bulk magnetization doesn’t stay out of alignment for long. Once the RF pulse is turned off, the magnetization returns to equilibrium in tenths to tens of seconds. As it relaxes, sensor coils detect the precessing magnetization. Applying small field gradients produces location-specific measurements that can then be used to construct an image. Nuclei in different tissues of the human body relax at different rates, so a particular tissue or organ can be targeted for imaging by applying certain sequences of specifically timed RF pulses. (For more on the physics of NMR and MRI, see Physics Today, December 2003, page 24
MRI signal strength scales approximately with the square of the magnetic field strength, so low-field instruments start at a big disadvantage. Longer scans would increase the signal-to-noise ratio and thus could yield clearer images. But during an examination, which typically takes less than an hour, a patient must lie in a confined tube-shaped area and during each scan remain motionless—any movements introduce artifacts into the final images. The longer the scan, the more likely it is that a patient will move.
A low-field instrument won’t make the examination time shorter, but it can be more comfortable for a patient. Because the permanent magnets don’t need to be cooled with liquid helium, they can be designed with an open geometry, so the machine may feel less claustrophobic for patients. The scanner designed by Wu and colleagues is pictured in figure
Figure 1.

This MRI scanner operates at 0.05 T and costs much less than a conventional 3 T instrument. It can be placed in rooms that don’t have expensive shielding, and its open design provides some level of comfort for patients. (Adapted from ref.

The more open design does have drawbacks. In addition to the RF noise that a patient might cause, low-field, unshielded MRI instruments are particularly susceptible to environmental sources of electronic noise such as computers and electric motors.
Extracting a signal
Wu and colleagues designed their MRI scanner without any RF shielding. Because it uses neodymium permanent magnets rather than a superconducting magnet, the device doesn’t require much energy; the entire scanner can be powered by a standard electrical outlet.
A 2021 paper by the same group reported the key hardware components of a relatively small MRI device that could take images of the brain. 3
To make the device capable of imaging not just the head, the researchers made a number of refinements to improve the magnetic field’s homogeneity and limit unwanted eddy current in the magnets. The device—which is large enough to fit a patient’s body between the top and bottom magnetic plates—is capable of imaging the head, heart, lungs, and abdominal area.
A lower-power machine, however, isn’t worthwhile if it can’t produce useful data. To get a clear image from an instrument with a weak signal and no shielding, the researchers first needed to understand how electromagnetic interference showed up in their signals. Using several coils placed around and inside the device, they measured both interference and the magnetic resonance signal during a normal scan and then measured only the interference when no magnetic resonance signals were collected. The data, in addition to high-quality images produced by high-field MRI instruments, were compiled to train an AI prediction algorithm that estimated interference-free MRI data. 4
The algorithm uses deep learning, which is a type of AI that’s loosely based on neural networks. It uses multiple classification layers to identify successively more complicated features in a data set. Because of advances in computing hardware and software, the method has become popular for all sorts of applications, including such complex tasks as predicting a protein’s 3D structure (see Physics Today, October 2021, page 14
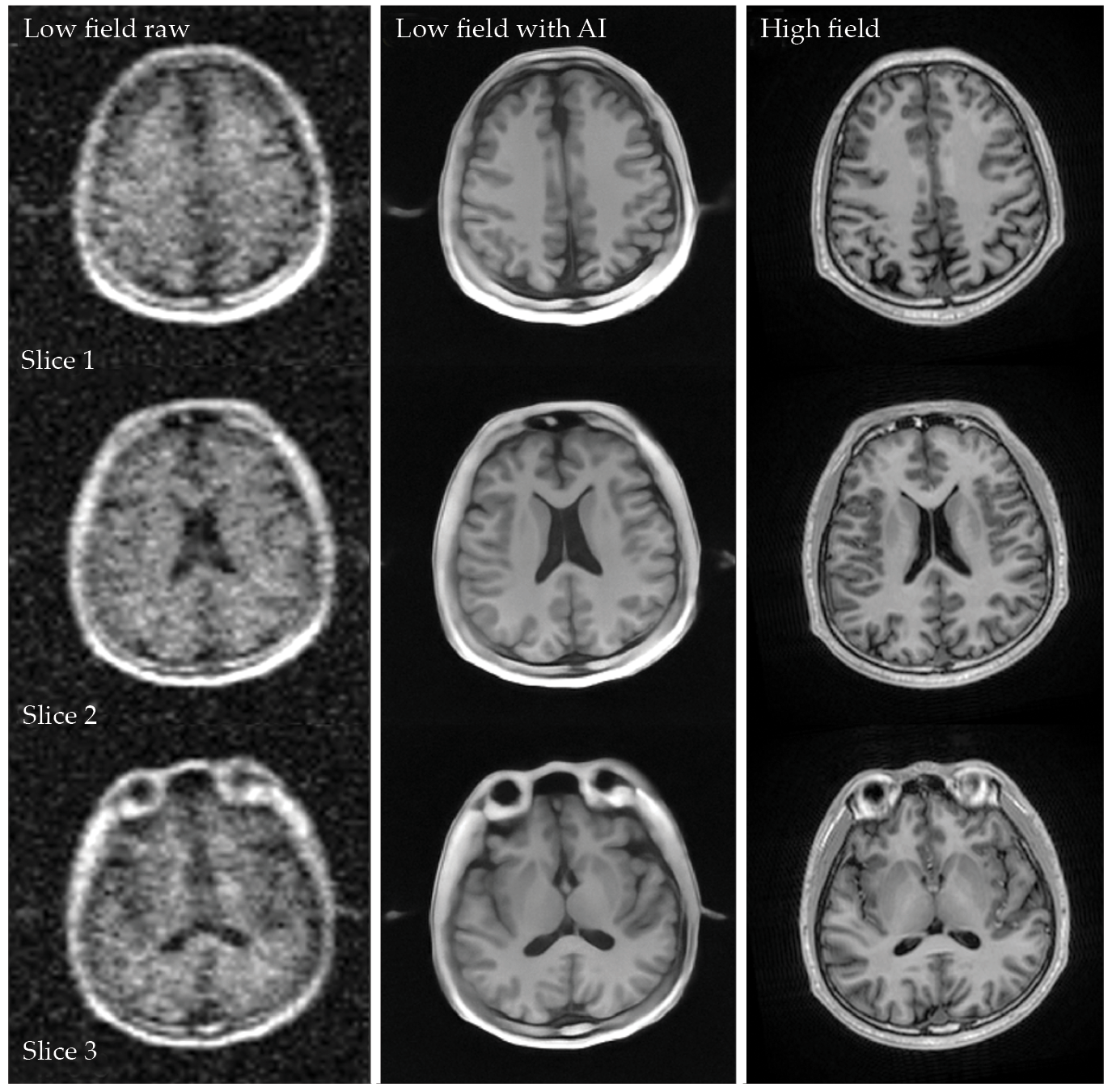
After training, Wu and colleagues’ AI model reduces noise artifacts in the low-field instrument’s images. Because the deep-learning algorithm is trained to identify the magnetic resonance signal, it can generate clean images even in a changing noise environment and without RF shielding. As shown in figure
Figure 2.

Artificial intelligence (AI) can reduce the noise and improve the spatial resolution of MRI. The left column shows image slices of a healthy human brain collected by a prototype 0.05 T scanner. The middle column shows the same images corrected with an AI deep-learning algorithm, and the right column shows results from a conventional 3 T scanner. Although some details are sharper in the high-field instrument’s images, the AI-reconstructed images show many of the same anatomical features. (Adapted from ref.
Wu and colleagues aren’t the first to use AI to enhance the image quality of low-field MRI instruments. Several previous approaches focused on identifying and correcting for electromagnetic interference to improve brain MRI. 5 Unlike previous small devices, the one developed by Wu and colleagues is large enough to clearly image anatomical structures from multiple areas of the body.
Although the new results are improved, the low-field images and the high-field images do have differences—as seen, for example, in some of the smaller, darker features at the edge of the brain in figure
Expanding MRI access
Wu and colleagues have begun some clinical evaluation. In two papers published last year, Wu’s group reported that their low-field scanner revealed the same lesions in the brains of stroke patients as did a 3 T device. 4 , 6 Wu and others in the MRI community are working to determine the clinically relevant details that low-field MRI can identify and those it can’t. “We need to improve the raw data quality as well as AI models,” says Wu. “Both areas are still unsettled but full of hope, in my view.”
Expanded MRI access is a big goal of the community, and low-field devices could help, if they’re approved for broad imaging applications. Wu and colleagues estimate that if manufactured at an industrial scale, hardware material for their device would cost about $22 000. A reconditioned 1.5 T machine costs roughly 10 times as much, and a brand-new 3 T machine may be between $2 million and $3 million. The construction and installation expenses for an RF-shielded room can raise the price tag by a few million dollars more.
Both high-field and low-field machines need regular maintenance and repairs, so the total expense of the instrument developed by Wu and colleagues would be higher than the hardware cost. Still, the choice to use a permanent, low-field magnet and to forgo any RF shielding makes it far more affordable than a conventional, high-field MRI machine.
Because the low-field machine is small and doesn’t need RF shielding, it could be useful in places that usually don’t have an MRI machine, such as in an emergency room. Underserved communities in the rural US or other places worldwide would benefit from more MRI access. The most common type of liver cancer, for example, affects roughly 1 million people globally each year and is the fourth leading cause of cancer-related death worldwide. 7 If doctors could diagnose the disease at an earlier stage with the help of an affordable MRI scanner, a patient’s prognosis could be improved.
References
1. U. C. Anazodo et al., NMR Biomed. 36, e4846 (2023). https://doi.org/10.1002/nbm.4846
2. Y. Zhao et al., Science 384, eadm7168 (2024). https://doi.org/10.1126/science.adm7168
3. Y. Liu et al., Nat. Commun. 12, 7238 (2021). https://doi.org/10.1038/s41467-021-27317-1
4. C. Man et al., Sci. Adv. 9, eadi9327 (2023). https://doi.org/10.1126/sciadv.adi9327
5. S. A. Srinivas et al., Magn. Reson. Med. 87, 614 (2022). https://doi.org/10.1002/mrm.28992
6. V. Lau et al., Magn. Reson. Med. 90, 400 (2023). https://doi.org/10.1002/mrm.29642
7. J. M. Llovet et al., Nat. Rev. Dis. Primers 7, 6 (2021). https://doi.org/10.1038/s41572-020-00240-3
More about the authors
Alex Lopatka, alopatka@aip.org





