Homemade panels significantly reduce noise in a busy hospital unit
DOI: 10.1063/1.2774087
Hospitals are noisy. Pagers bleep, loudspeakers blare, equipment hums, visitors chatter. In that constant din, staff have to communicate and patients have to recover. Quieter hospitals would bring relief to all their inhabitants.
Over the years, the World Health Organization (WHO) and other bodies have recognized hospital noise as a problem and set standards in the hope of mitigating it. But in hospitals, saving lives and treating patients top all other priorities.
Walls, floors, and other surfaces must be kept germfree, which means they must be easy to clean. The smooth, hard materials that abound in hospitals reflect sound around corners and doorways. Powerful, usually noisy, ventilation systems are needed to filter, cool, and heat the air. Alarms and pagers have to alert staff wherever they are, whatever they’re doing.
Despite the obstacles to tranquility, reducing hospital noise is feasible. In a recent paper, Ilene Busch-Vishniac and James West of the Johns Hopkins University in Baltimore, Maryland, and their students have demonstrated a simple and effective solution: Install fiberglass-filled panels on walls and ceilings. 1
The installation of panels is the latest milestone in a project that began almost by chance four years ago. Each unit of the Johns Hopkins Hospital (JHH) has an advocate on the hospital’s administrative staff. For the pediatric intensive care unit, the advocate’s role is served by Stephanie Reel, the hospital’s chief information officer.
One day, when Reel was touring PICU, the staff complained to her of the noise. Reel knows Busch-Vishniac, who was president of the Acoustical Society of America at the time, and asked her to help.
Busch-Vishniac and her colleague West expected the request would take a few hours to fulfill. All they needed to do, they presumed, was walk through the unit, assess the noise, then trawl the literature for the most appropriate and effective mitigation methods.
To Busch-Vishniac and West’s surprise, few studies of hospital noise had been published in the open literature. Papers on noise mitigation were even harder to find. When planning a new hospital, administrators tend to hire professional consultants whose reports and recommendations are not easily accessible.
What studies Busch-Vishniac and West could find yielded a troubling picture. No hospital in any of the studies met the WHO standards. Worse, the trend is upward: Hospitals are getting noisier.
Never really quiet
The two researchers decided to undertake their own study. With the support of the JHH administrators and staff, they set about assessing the noise in different hospital units. So far, they’ve taken measurements in seven: two pediatric units, two cancer units, two surgical units, and an emergency room. Detectors were placed at various locations within each unit, including operating theaters, nurses stations, patient rooms, and hallways. Two properties were monitored throughout the day: sound level and frequency spectrum. In some locations, they also measured reverberation time.
Busch-Vishniac and West presented their results in a series of four papers. No unit was ever really quiet. Figure 1 shows one measure of sound level, L eq, calculated over 10-minute intervals and averaged across units for various locations (see the

Figure 1. Sound levels in hospital units vary throughout the day depending on location within the unit. Empty patient rooms experience the most fluctuation and are the quietest. Hallways, occupied patient rooms, and nurses stations experience less fluctuation and are noisier. Each point represents the equivalent power L eq in 10-minute intervals averaged across five different hospital units.
(Adapted from ref. 2.)
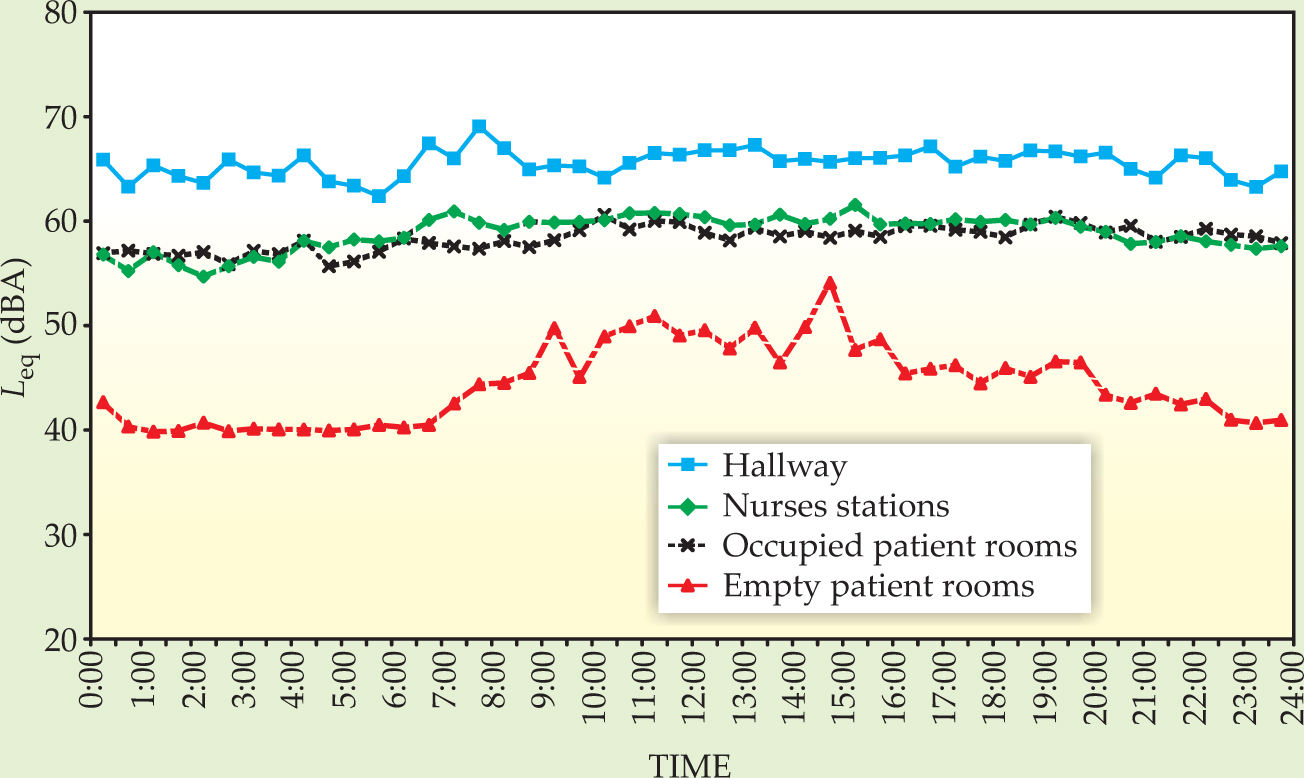
The quietest places were the empty patient rooms, but they’re hardly quiet. At night, the L eq settles at a value of 40 dBA, which corresponds to a loud whisper. The hallways are never quiet. There, the L eq of about 65 dBA corresponds to loud conversation or moderate automobile traffic.
Figure 1 suggests that people are the main source of noise, given that the noisiest places are where humans are present most of the time. That suggestion is borne out by the spectrum of the noise, which, like human speech, is a slowly falling function of frequency. The spectrum is augmented at the low-frequency end by HVAC noise and at the high-frequency end by what the JHU team suspect is the bleeping of pagers and alarms.
The JHU team measured reverberation because it helps to characterize how clearly speech can be perceived. Multiple reflections smear out sharp enunciation. To offset that effect, speakers in reverberant rooms strive to make themselves understood by speaking louder, which worsens the acoustic environment. In their investigations, Busch-Vishniac and West found reverberation times of about 1.2 s, which is considerably higher than the 0.6 s set five years ago in ANSI S12.60-2002, American National Standard Acoustical Performance Criteria, Design Requirements, and Guidelines for Schools.
Toward a solution
Having measured noise, Busch-Vishniac and West set about reducing it in perhaps the most demanding of the units they investigated: Weinberg 5C, a ward for sufferers of leukemia and other blood cancers. The patients in Weinberg 5C receive chemotherapy, which compromises their immune systems and severely constrains what materials can be introduced into the unit.
Acoustic tile, whose foamy surface could harbor germs, is off limits. Indeed, the health and safety requirements of hospitals are so stringent that Busch-Vishniac and West opted to create noise mitigation methods out of materials already approved. Fortunately, among those materials is an excellent sound absorber: fiberglass insulation.
Unwrapped and exposed to air, the fluffy fiberglass fibers would be unacceptable. The JHU team wrapped the material in a commercial, bacteria-killing fabric to create soft, floppy panels. Aluminum foil provides the backing and industrial-strength Velcro the means of attaching the panels to the walls and ceilings without the disruption of drilling holes.
As for where to install the panels, they picked the two locations that appear noisiest in figure 1: the nurses station and the hallways. The nurses station was especially bad, in part because of the focusing effect of a domed ceiling. Figure 2 shows the ceiling and the newly installed panels.

Figure 2. The nurses station in the Weinberg 5C cancer unit of the Johns Hopkins Hospital features a domed circular ceiling. Despite its visual charm, the dome worsens the noise levels. The installed panels reduced the sound level and reverberation time.
(Adapted from ref. 1.)

Installing the panels reduced the noise level by about 6 dBA and the reverberation time from 1.2 s to 0.4 s. Perhaps more important, patients and staff noticed the improvement and reported their impressions in surveys. For example, before the panels were installed, 50% of Weinberg 5C nurses strongly agreed with the statement “Noise makes it difficult to hear conversation.” After the installation, that proportion dropped to 17%.
Further gains are clearly possible. For one thing, the antibacterial fabric impairs the sound-absorbing effect of the fiberglass stuffing. The fabric was bought off the shelf without regard to its acoustical properties. A better choice might improve the panels’ performance. Their placement could also be optimized.
One reason why sound mitigation has received little attention is that the din is tolerable. Even though doctors and nurses rely far more on oral communication than other workers do, they still manage to communicate. Humans are especially adept at extracting audible signals from a noisy background.
Oral communication has its limitations. With a handheld device equipped with voice recognition, a doctor could dictate a drug regimen and then transmit it to a unit’s entire nursing staff, not just to the nurses within earshot. But voice recognition machines require a far higher signal-to-noise ratio than human ears do. If such gains in communication efficiency are to be realized, hospitals must become quieter—which would benefit the humans as well as the machines.
Characterizing and measuring sound
Human ears can detect sound over an astonishing range of intensity. Audibility starts at a mean air pressure of 20 µPa and extends through 13 orders of magnitude to reach the onset of pain at 100 MPa. To cope with that range, our sense of hearing responds logarithmically to increases in pressure. And for that reason, acousticians find it convenient to measure sound levels as perceived by humans in decibels.
By definition, the sound level in decibels is 10 log (P/P 0). Here, P is the acoustic power and P 0 is a reference power, usually given as the threshold of audibility. In hospitals, factories, and other noisy environments, the intensity of sound tends to fluctuate strongly on a variety of time scales. To characterize the intensity, acousticians record minimum and maximum levels as well as the equivalent power, L eq, which corresponds to the mean power measured over a specified interval, say, 10 minutes. (The averaging takes place before the log is taken.)
The frequency range our ears can pick up, 20 Hz to 20 kHz, is also wide enough that our hearing responds logarithmically. Ranges of pitch are typically given in octaves, each spanning a factor of two. The sensitivity of our ears as a function of frequency is not flat. Sound-measuring devices incorporate a filter that mimics the ears’ frequency response. To indicate the filter’s use, acousticians append an A to the decibel symbol.
References
1. M. MacLeod, J. Dunn, I. J. Busch-Vishniac, J. E. West, A. Reedy, J. Acoust. Soc. Am. 121, 3501 (2007). https://doi.org/10.1121/1.2723655
2. I. J. Busch-Vishniac, J. E. West, C. Barnhill, T. Hunter, D. Orellana, R. Chivukula, J. Acoust. Soc. Am. 118, 3629 (2005). https://doi.org/10.1121/1.2118327




