DARPA joins industry, academia to build better prosthetic arms
DOI: 10.1063/1.2364231
Body armor is saving the lives of US troops in Iraq and Afghanistan. At the same time, though, it’s leading to a whole new range of head and limb injuries in people who previously would not have survived, says Geoffrey Ling, program manager at the Defense Advanced Research Projects Agency. Upper-body injuries, in particular the loss of hands or arms, have become more common; each week in Iraq, several American troops lose a limb. To improve the lives of these young amputees, DARPA has launched a two-phase, four-year, $70 million research program to build a better prosthetic arm.
“The idea is to develop a prosthetic arm whose hand can grasp and throw a baseball, play the piano, or pick up a flower and place it in a vase as naturally as a biological arm,” says Stuart Harshbarger, a biomedical engineer at Johns Hopkins University’s Applied Physics Laboratory outside Baltimore, Maryland. “These are tasks that are too difficult for the current generation of prosthetic limbs.” The APL-led project involves more than 30 organizations and research groups from government, academia, and industry, and includes leading prostheses developers, neuroscientists, engineers, and related researchers.
A helping hand
The first phase of the project is split into two parts. DEKA Research and Development Corp in Manchester, New Hampshire, got $18.1 million to turn current state-of-the-art limbs into commercial products. Meanwhile, APL’s biomedical business division has $30.4 million to map out areas of research to develop prosthetic arms with extensive neural control.
The so-called phase-one prototypes will be modular, so they can be used by amputees who have lost a hand, a portion of the arm below or above the elbow, or the entire arm. Modern-day prostheses are attached externally, but future ones may connect directly to the human skeleton via a surgically created socket. The most sophisticated artificial arms today cost $90 000 on average, and although future models will still need to be custom-made, standardization should make them less expensive. In two years, if DARPA is satisfied with APL’s progress, the lab will get an additional $24.4 million toward the project’s second phase, which aims to create a comfortable and lifelike robotic arm that looks and acts like a normal limb, including the way it transmits temperature and sensory data to the brain.
Research on upper-limb prostheses is far behind lower limbs, says Kevin Kelley, the project liaison for Otto Bock Health Care, a leading prosthetics provider based in Austria. About 80% of the 1.8 million amputees in the general US population have lost lower limbs, mostly from diabetes and strokes. Younger patients lost limbs mainly through accidents and war injuries. “We’re still servicing some wooden hands designed in the World War I era,” says Kelley. The DARPA project “is something the private sector would never have been able to do on its own,” he adds.
The pivoting and moving of joints by the human arm and hand combined can be described in 22 degrees of motion. Arm and hand amputees can currently choose among pincers, claws, and nonfunctional cosmetic prostheses. More sophisticated models require a series of pulleys and levers to move an arm, and the latest versions use brushless motors and gear trains to move through three degrees of motion. These artificial limbs, which are attached to the body by a Velcro vest, are not popular. “Patients perceive these models as a heavy, dead weight and the three degrees of motion cannot be performed simultaneously, so the movements are not natural,” says Kelley. “There is no sensory feedback, so the wearer can’t perceive when the limb is touching or manipulating something except visually. For all these reasons many patients are not motivated to use them.”
The human hand in particular is “so dexterous and sensitive that people can read Braille, but [it] also has an extraordinary strength of grip,” Kelley says. “Trying to replicate that performance is really quite a challenge.” The hand can support a significant amount of weight, and it transmits massive amounts of sensory data to the brain. The best current prosthetic hands can only open and close in a pincer fashion. Proto 2, the new APL prototype hand being developed for delivery in 2007 (see the cover image of this issue) will have a mechanical frame and will be coated in silicone to give the look of a natural hand. The prosthetic hand will contain 22 joints controlled by 11 tendons, along with pressure-, vibration-, joint-, and heat-sensing capabilities controlled by the wearer’s neural system. “This prototype will weigh no more than a human hand, will act like one, and can manipulate a ball whether it is fragile like an egg, hard like a pool ball, or spongy,” says Tom Van Doren of New World Associates, Human Systems Group, a Proto 2 subcontractor based in Fredericksburg, Virginia.
Neural controls
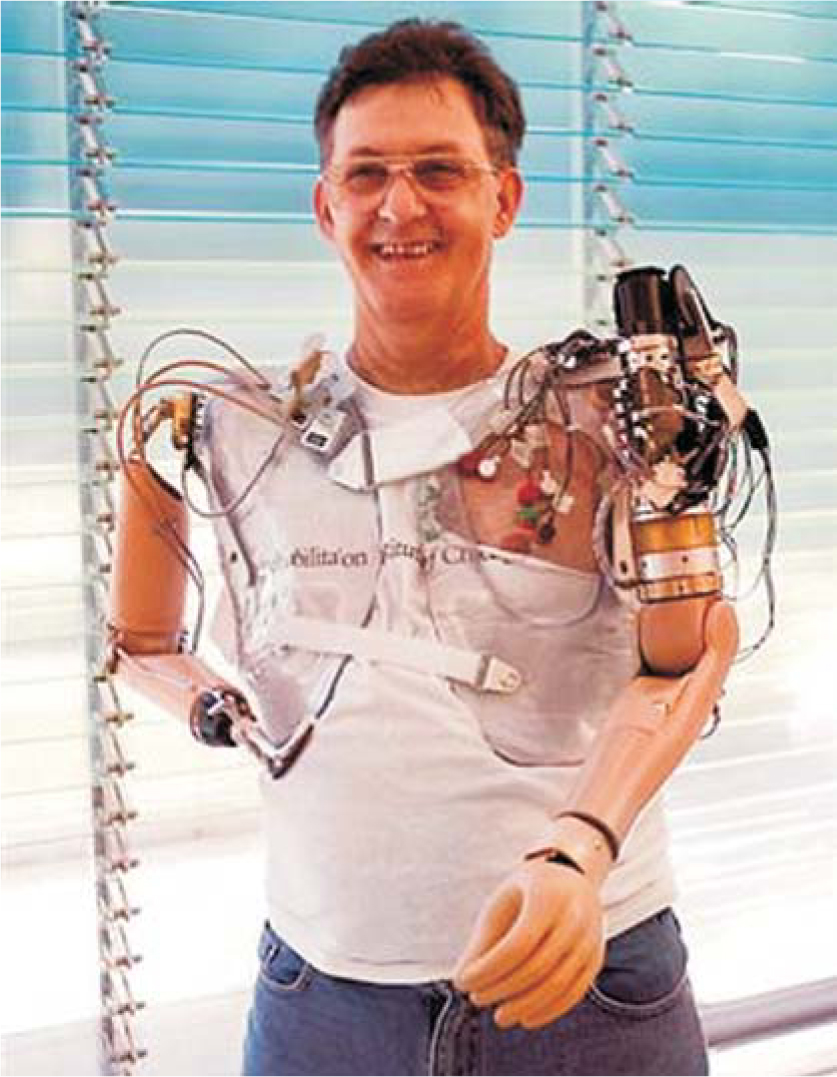
Some research groups participating in the DARPA prosthetic-arm project have already started experimenting with neural controls. As shown on the next page, Jesse Sullivan, who had both arms amputated after suffering electrical burns five years ago, sports a traditional pincer and a myoelectric hand in a hybrid prototype system that was developed by Northwestern University Prosthetics Research Laboratory (NUPRL) and the Rehabilitation Institute of Chicago (RIC). He underwent surgery on his left side to transfer nerve endings from what remains of his shoulder to the pectoral muscles on his chest. The nerves grew into the muscle and now transmit thought-generated impulses to mechanically control a prosthetic arm. To close his hand, for example, Sullivan imagines the movement, causing the transplanted nerve endings in his chest to twitch, a signal that, in turn, is picked up by electrodes in his prosthesis and sent to his hand, which closes.
Sullivan’s prosthetic arm has seven degrees of motion and more closely mimics a human arm than standard prosthetics (for a movie demonstration, see Physics Today’s online version of this story). He can take out the garbage, shave, and put on his socks, but he does not have the dexterity to tie his shoes, pick a flower, or throw a ball. His prosthesis is also cumbersome and expensive—$100 000 not including surgery—and requires frequent maintenance.
In the short term, to gain better user control over prosthetic arms, APL is looking into combining RIC’s technique with sophisticated pattern-recognition algorithms to “guess” the user’s intent from the limited nerve signals and preshape the hand to grasp objects, for example. For the long term, cortical neural interfaces, in which neural impulses to and from the brain are intercepted for direct communication with the prosthesis, and peripheral neural interfaces appear to be better bets. “It’s a challenging part of the project, but cortical plasticity could be the key. We need to train the limb and the user to both respond to mistakes and learn from them,” says APL’s James Beaty. “Once installed, the system has to work in real time.”
APL is also creating virtual-reality simulations for patients to learn how to control their artificial limbs. “We need to get to the point that when someone is pushing against a virtual table, it feels like a table to the user,” says APL’s James Burck, a systems engineer.
Another approach is to use injectable myoelectric sensors (IMES). Partners in the APL team at NUPRL and at Sigenics Inc of Lincolnshire, Illinois, are developing centimeter-long devices that can be implanted in residual muscles to record and amplify small nerve signals directly from activated muscles. Researchers at the University of Utah and elsewhere are developing miniature recording systems to access the body’s inherent neural signals for control of the prosthetic limb. These efforts will make the small neural signals naturally transmitted to the human hand and the limb more readable, Harshbarger says.
Power problems
“Once you have your next-generation artificial limb, you still have one major problem,” says Harshbarger, “how to power it.” Whereas traditional prosthetic arms are maneuvered with body motion, DARPA’s first prototype will be battery-powered, like the state-of-the-art limbs today, and future versions may rely on fuel cells or small cartridges of hydrogen peroxide—which could be jettisoned and replaced almost as easily as a flashlight battery. “We’re also looking to see whether body movement could power the small sensor components and whether highly efficient hydraulic pumps could be used [to move the limb],” says Harshbarger. Current prosthetic arms can lift a maximum weight of about 9 kilograms. DARPA hopes to raise that to 27.3 kg, which requires stronger, more efficient motors and more power. The arm and hand for Proto 2, weighing 3.2 kg itself, can manipulate 22 kg. “This is unprecedented for robotic arms,” says Van Doren.
DARPA plans to make design decisions about the phase-one prosthesis in November 2007. In the end, says Harshbarger, “DARPA may decide that [the APL team] should build an arm with 15 to 18 degrees of motion and less strength that could potentially cost less per system than our initial prototypes might. These are the kinds of system tradeoffs that will be addressed as we prepare the system integration plan for transition to phase two.” In the meantime, no one is forgetting how beneficial even a minor improvement will be for the injured troops. Says Harshbarger, “I’ve never been on such an extremely rewarding project in which so many research groups have set aside their competitiveness with each other to work towards the common good.”

Electrodes on one side of double-amputee Jesse Sullivan’s chest pick up thought-generated signals from his nerves to control a state-of-the-art prosthetic arm. His other arm is an old-fashioned pincer.
REHABILITATION INSTITUTE OF CHICAGO

A well-worn prosthetic arm. Some users prefer an old basic design, like this one, rather than a more modern device.
OTTO BOCK HEALTH CARE

More about the authors
Paul Guinnessy, American Center for Physics, One Physics Ellipse, College Park, Maryland 20740-3842, US . pguinnes@aip.org





