Wireless sensors for the tiniest patients
DOI: 10.1063/PT.3.4197
If you’ve ever been a hospital patient, you’re likely familiar with the experience of being hooked up to a tangle of wires and sensors. Despite advances in technology, the basic setup hasn’t changed much in 50 years: Rigid sensors are held against the body with mechanical clamps or strong adhesives, and they’re connected by wires to an external box of electronics that processes the signals. The sensors are necessary to monitor your vital signs. But they restrict movement—you can’t get up from your bed without assistance—and they’re uncomfortable.
The problems are compounded for hospitalized newborns, especially those born prematurely. The skin of infants born at less than 32 weeks’ gestation can easily be traumatized by the harsh adhesives. More than 90% of children born prematurely bear scars later in life from their early hospitalization. Not all of those are from the sensors, but many are.
Wired sensors also get in the way of bedside care such as feeding, bathing, and diaper changing. And they inhibit crucial interactions between babies and their parents. Cuddling a new baby is an emotional experience, of course, but skin-to-skin contact also carries real medical benefits: It stabilizes the baby’s heartbeat and body temperature, promotes feeding and weight gain, and ultimately paves the way for a shorter hospital stay. 1
Researchers at Northwestern University are working toward obviating the drawbacks of wired sensors. The project is led by materials and electronics engineer John Rogers, pediatric dermatologist Amy Paller, and physician-engineer Shuai Xu, formerly a postdoc under the joint mentorship of Paller and Rogers but now in charge of coordination between the medical and clinical halves of the team.
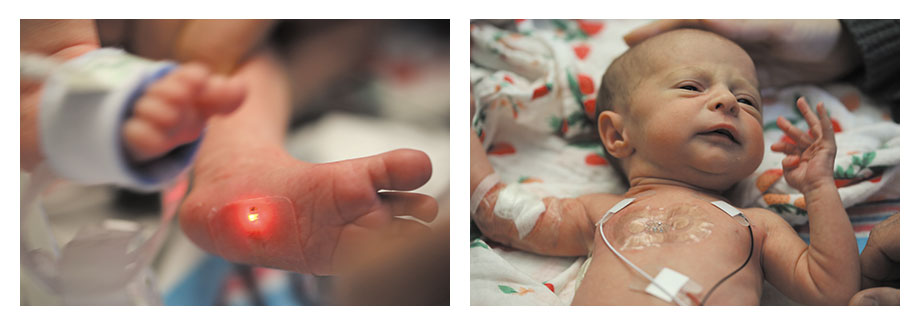
The researchers have created a system of two flexible, wireless sensors, shown in figure
Figure 1.

Just two wireless sensors, one on the foot and one on the chest, suffice to monitor all of an infant’s vital signs. But until the wireless devices are approved for use on their own, test patients need to wear the standard wired sensors too.
NORTHWESTERN UNIVERSITY
Cutting the cords
Rogers and his engineering colleagues have been developing flexible, stretchable, skinlike electronics for more than a decade. (See Physics Today, May 2008, page 84
Three years ago, Paller attended a talk at which Rogers spoke about his flexible electronics work, and she realized they had the potential to meet a pressing need in neonatal intensive care units (NICUs). She’d worked with him before on sensors to monitor wound healing, and a new branch of their collaboration was born.
The conventional system for monitoring a newborn’s vital signs uses five wired sensors. One is a simple adhesive-backed temperature probe. Three are electrodes that together record an electrocardiogram (ECG), which monitors the speed and regularity of the heartbeat. Because the heart signals look different when the lungs are full, the ECG also provides a measure of respiratory rate.
The final sensor records a photoplethysmogram (PPG), an optical measurement of blood flow. If you shine a flashlight through a thin part of your flesh, you’ll see the transmitted light tinged with red from your blood. If you could gauge its intensity precisely enough—and especially if you could see in the IR—you’d see it pulsate with each beat of your heart. From the oscillation amplitudes at different wavelengths, you could determine your blood oxygenation level, a measure of how effectively you’re breathing. In adults, a PPG sensor is often clamped onto a finger. In infants, it’s taped around the foot.
The building blocks more or less existed to reproduce all those functions wirelessly. For example, sensors could transmit data via near-field communication (NFC), an offshoot technology of RFID that’s used in contactless payment schemes. Electronics can also be powered wirelessly, thereby obviating the need for bulky batteries.
The hard part was in putting all the pieces together into a device that would meet the stringent requirements of the NICU. Says Paller, “We spent two years just doing and redoing,” testing different materials, layouts, electronic designs, and algorithms for the sensors, in search of the ones that could operate continuously and reliably. “We couldn’t have any risk that they would fall off or stop working.”
Design challenge
The system that Rogers and colleagues came up with combines an hourglass-shaped sensor placed on the chest, holding two electrodes for recording an ECG, and a rectangular sensor wrapped around the foot, holding red and IR LEDs and a photodiode for recording a PPG. Either of the silicone-encased devices could easily be equipped with a temperature probe, so the researchers added one to each. As a result, they could measure not only an infant’s core body temperature, but also the temperature difference between the core and the periphery of the body. That quantity isn’t monitored with the current system of wired sensors, but it could help to diagnose circulation problems.
Because the ECG and PPG both track the heartbeat, an integrated system that records them synchronously can also measure the time it takes for a pulse to travel from the heart to the foot, as shown in figure
Figure 2.

From the synchronous streaming of two measures of the heartbeat—an electrocardiogram recorded by a chest-mounted sensor and a photoplethysmogram measured by a foot sensor—clinicians can extract the pulse arrival time from the heart to the foot, a measure of systolic blood pressure. (Adapted from ref.
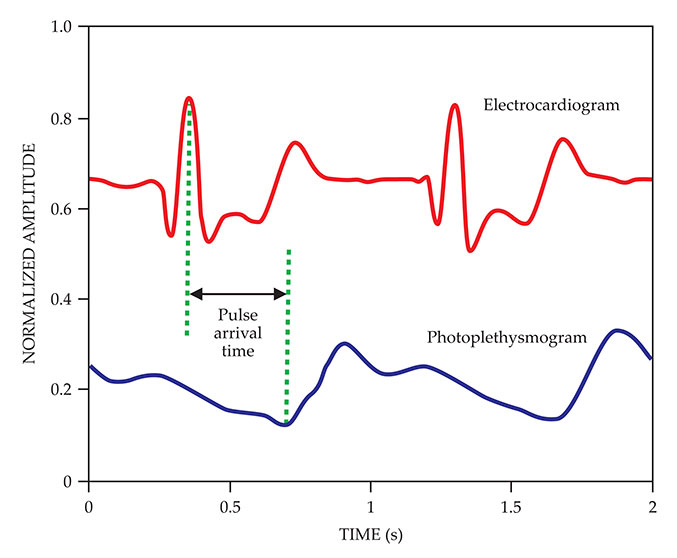
To reduce the amount of data that needs to be transmitted through the NFC link, the researchers designed circuitry to do much of the signal processing—for example, identifying the peaks in the ECG waveform—on the sensors themselves. The resulting signals don’t need expensive, specialized electronics; they can be streamed to any laptop, tablet, or smartphone.
The sensors are stretchy enough to function under strains of up to 16%, about the same as can be tolerated by skin. But stretching applies a shear force to the skin that can cause bruising. To mechanically decouple the electronics from the skin, the researchers added a thin fluid-filled layer to each sensor; the shear forces that remain are so slight they can’t even be felt. Even with the extra layer, the sensors are less than 300 µm thick.
The NFC link operates at a frequency, 13.56 MHz, that’s negligibly absorbed by biological tissues. The sensors are visually transparent, so doctors and nurses can tell at a glance if the skin underneath is becoming irritated. They’re waterproof and compatible with MRI and x-ray machines, so they can be left on while the babies are bathed or taken for routine imaging.
Clinical need
The wireless sensors have performed well in clinical trials so far, with no adverse effects on any of the patients. But before they can be approved by the Food and Drug Administration for general use in the US, more rounds of testing are needed to prove that they’re just as dependable as the current wired sensors. Until then, test patients must continue to wear wired sensors too.
While they’re waiting on FDA approval, the researchers have been working with hospitals in countries where mortality rates are high, even among full-term infants, due in part to a lack of diagnostic equipment. They have active pilot programs in several countries in Africa, and with grant funding from the Save the Children Fund and the Bill & Melinda Gates Foundation, they’ll be deploying their sensors to more sites in the developing world later this year.
Although the cost to hospitals in the US and elsewhere has yet to be determined, the researchers estimate that the wireless sensors could be mass-produced for less than $20 each. That’s less than hospitals currently pay for a set of adhesive-backed leads and connectors that are thrown away after a single use.
Older children and adults can also use the sensors—indeed, the first round of tests was on healthy adult volunteers. “We focused on the NICU because that’s where the clinical need was the greatest,” says Xu, “but I also see opportunities for the elderly or for burn victims with compromised skin.”
References
1. A. L. Jeffries, Paediatr. Child Health 17, 141 (2012). https://doi.org/10.1093/pch/17.3.141
2. H. U. Chung et al., Science 363, eaau0780 (2019). https://doi.org/10.1126/science.aau0780
3. D.-H. Kim et al., Science 333, 838 (2011). https://doi.org/10.1126/science.1206157
More about the authors
Johanna L. Miller, jmiller@aip.org