Slow but steady progress seen for carbon-ion cancer therapy
DOI: 10.1063/PT.3.5078
Decades after adoption in Asia, and following several false starts, carbon-ion cancer therapy may finally be coming to the US. In May, Mayo Clinic broke ground in Jacksonville, Florida, on a facility that will produce beams of carbon ions to treat cancer tumors.
The new center, which will also offer proton and conventional x-ray therapies, is expected to treat its first patients with carbon-ion beams in 2027, says Chris Beltran, chair of Mayo’s division of medical physics. Mayo will provide the estimated $233 million for the facility, and it has contracted Hitachi to build the synchrotron.
When the Jacksonville center opens, the US will have completed a circle that began with pioneering clinical trials in the 1970s at Lawrence Berkeley Laboratory’s Bevalac heavy-ion synchrotron. Led by Joseph Castro of the University of California, San Francisco, those trials established the safety and biomedical activity of carbon beams. Yet that work ended before trials of the treatment’s efficacy when the Department of Energy shut down the Bevalac in 1993.
Japan took notice of the research, opening the first of that nation’s seven carbon-ion therapy facilities in Chiba in 1994. Europe’s first carbon-ion therapy center, located in Heidelberg, Germany, began treating patients in 2009 (see Physics Today, June 2015, page 24

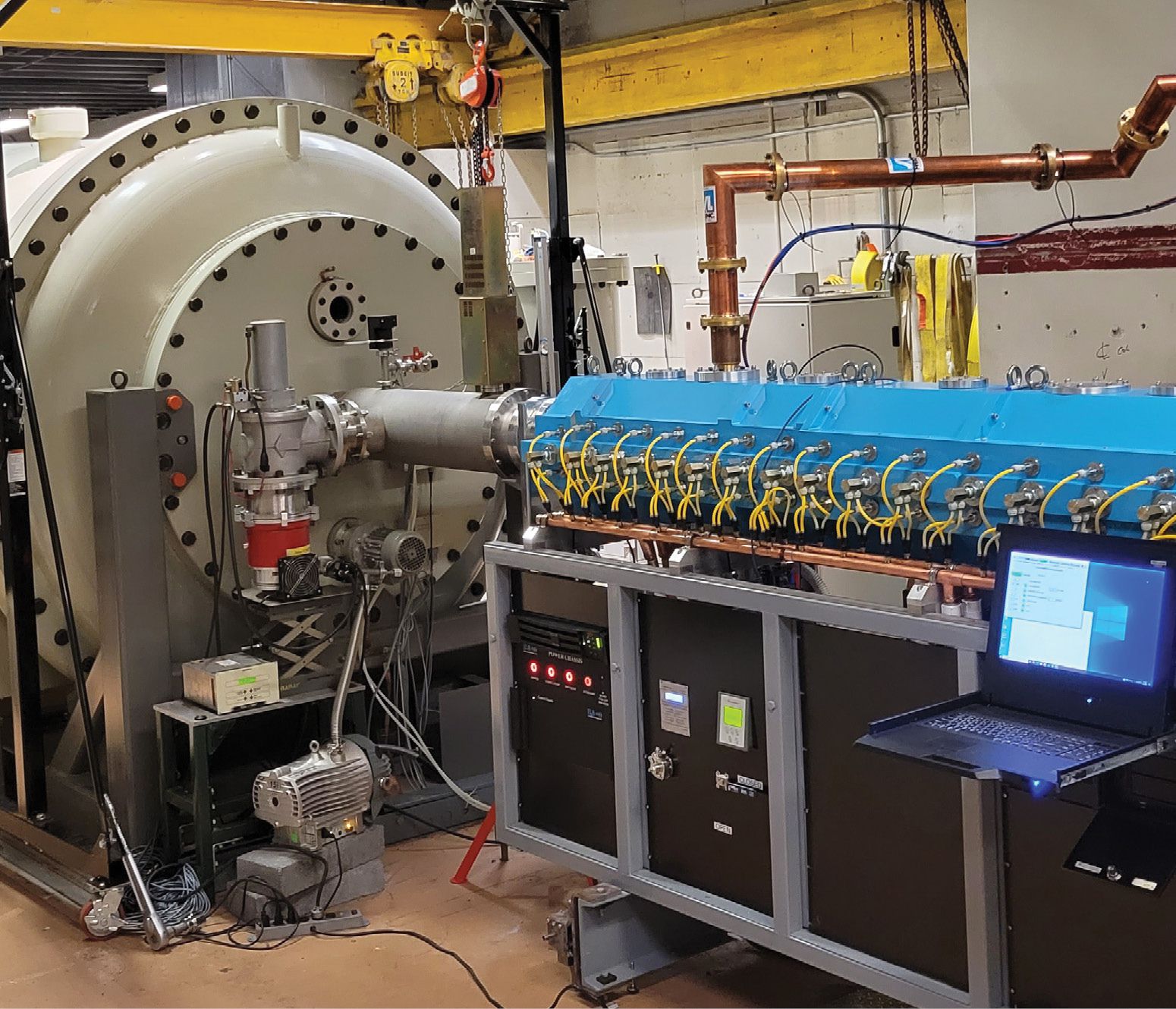
A linac booster (blue) attached to the end of the existing linac at Columbia University’s Radiological Research Accelerator Facility has become the first instrument in the US dedicated to research on heavy-ion radiation therapy. Installed earlier this year, the booster doubles the energy of the particles coming out of the linac and triples their range in tissue, university officials say. It will be used in preclinical research.
NARESH DEOLI/COLUMBIA UNIVERSITY
Five other centers are under construction—two in South Korea and one each in China, France, and Taiwan—according to the Particle Therapy Co-operative Group, a nonprofit organization that promotes the science, technology, and clinical application of particle therapy. China has another facility in the planning stage.
Plans for at least three other US carbon-ion treatment projects have stalled over the past decade. Before the start of the COVID-19 pandemic, the University of Texas Southwestern Medical Center (UTSW) completed the design for a treatment center in Dallas, selected Toshiba as the vendor, and was prepared to break ground in 2020. Hak Choy, a since-retired UTSW radiation oncologist who was the project’s chief proponent, says he had organized an international clinical trial that would have had patients travel to Japan and Italy for treatment. But UTSW management balked at the expense, fearing that hospital revenues would plunge during the pandemic, he says. “It is a risky project from the university’s point of view, because there is no guarantee of reimbursement [by Medicare, Medicaid, and insurers],” he says. “It’s not clinically proven, but there is a physics theory and biological theory for why it is beneficial.”
UC San Francisco had also proposed a center and, like UTSW, received a planning grant in the mid 2010s from the National Cancer Institute (NCI) to pay for design efforts.
Best Medical International, a privately held manufacturer of radiation oncology equipment, has been working with Brookhaven National Laboratory since 2012 to develop a carbon-ion therapy system, through cooperative R&D and technical-assistance agreements. Krishnan Suthanthiran, Best Medical’s president, says he still expects a system to be ready for installation in two years, possibly at a Best-owned property in Pennsylvania.
Chicken and egg
In addition to the prohibitive expense, a major impediment to carbon-ion therapy in the US is the lack of published evidence for its benefit over other forms of radiotherapy. “Despite being out there for 20 or 30 years, there’s not a document or a clinical practice … where I can say if you have prostate or breast cancer, then this paper says you should get carbon,” says Jeffrey Buchsbaum, the medical officer in the clinical radiation oncology branch at NCI. “There is a lack of peer-reviewed literature in robust, random trials,” which are the standard in the US.
Yet despite a similar lack of published randomized clinical trials comparing proton therapy to conventional x-ray therapy, the US has broadly accepted proton therapy. The first proton-therapy center in the US, at Loma Linda University Medical Center in Southern California, opened in 1990, with support from a congressional earmark. Today, the US leads the world in the number of proton facilities, with 41, according to the Particle Therapy Co-operative Group. A half dozen NCI-sponsored and other randomized trials on proton therapy are nearing completion or publication.

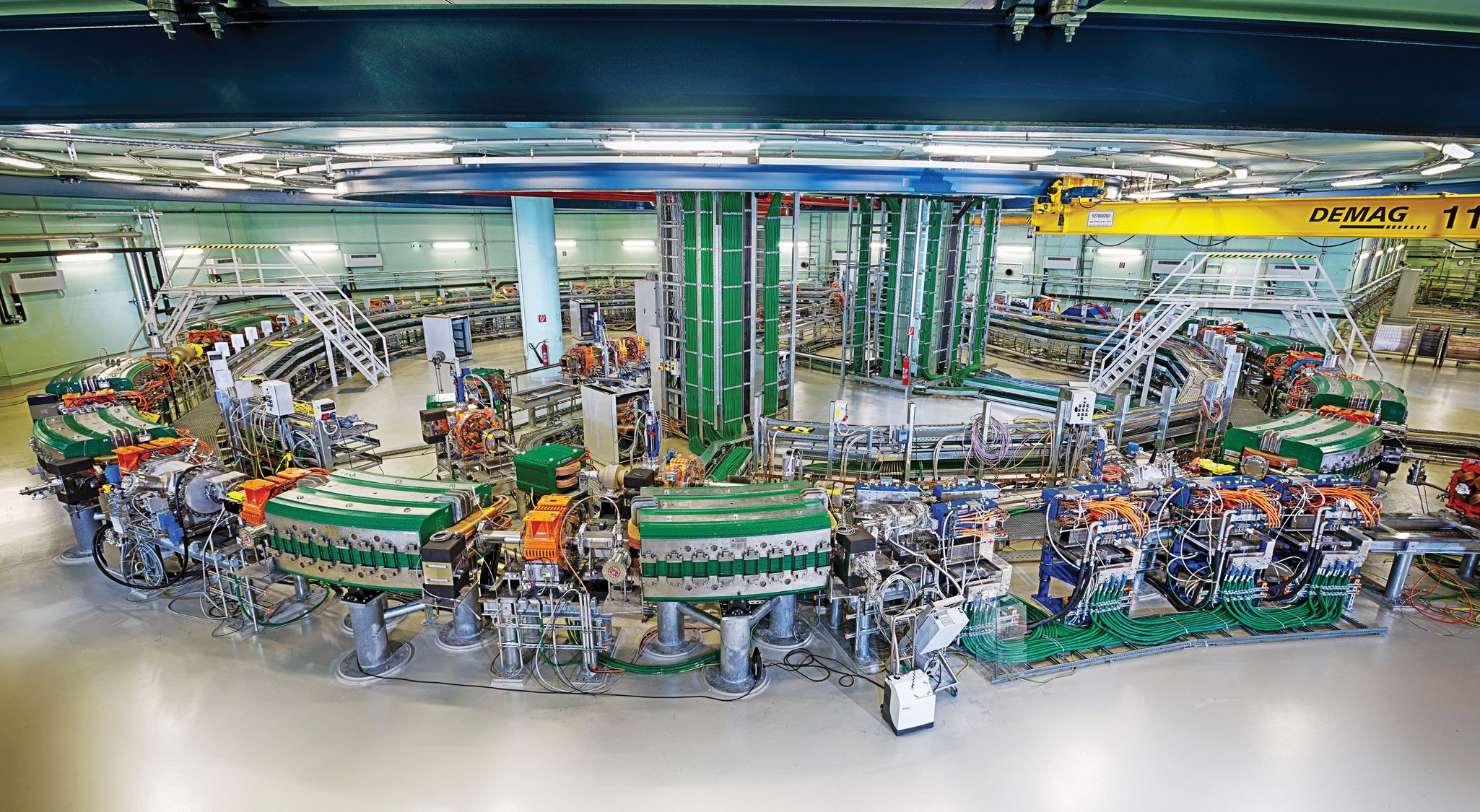
The synchrotron at MedAustron, a proton and carbon-ion cancer therapy center in Wiener Neustadt, Austria. Carbon-ion energies range from 120 to 400 MeV, and proton energies of 60 to 250 MeV are available. The higher the particle energies, the greater the beam’s penetration depth into the body.
KAESTENBAUER/ETTL
Mayo Clinic is moving forward on the Jacksonville facility without assurances of regulatory approval. Beltran says it’s hoped that the Food and Drug Administration will look at all the data and methods that have been used elsewhere. “Hopefully we can leverage the published research for FDA clearance and do more clinical trials going forward.” Approval under an investigational-device exemption allows devices to be used in a clinical study to collect the safety and effectiveness data needed to support a premarket approval application and subsequent approval stages.
Without full regulatory approval, public and private health insurers are unlikely to pay for carbon-ion treatment. But hospitals will need operating revenues to pay off the loans they take out to build facilities. In Germany, the government paid half of the €120 million ($122 million) cost of the Heidelberg center. As the first in the country, Heidelberg was able to arrange agreements with insurers to pay for clinical trials, says Oliver Jäkel, head of the division of medical physics in radiation oncology at the German Cancer Research Center. The loan was paid off in seven years.
Considerable in vitro evidence shows that carbon therapy works, says Jäkel, but randomized clinical trials are difficult because of the length of time required to obtain meaningful data, around 10 years. Criteria for inclusion in trials is highly specific, and many trials don’t conclude, because the number of patients is insufficient. Although centers could work better together, he says, there still aren’t enough of them to supply a sufficient number of patients.
Joseph Lidestri, a physicist and engineer at Best Medical, says Japanese scientists haven’t been given proper credit for the clinical research they have done with carbon ions, even if their trials haven’t been randomized. “They did all the hard work for the last 30 years, and you have people who want to mystify carbon therapy and say we don’t know enough yet. You just have to look hard, and you’ll find it.”
David Brenner, director of the Center for Radiological Research at Columbia University Medical Center, says he’s been motivated in his research on heavy-ion therapy by the results from Japan on treating pancreatic cancer with carbon ions. Noting that survival rates for that cancer type, typically 25% to 30%, haven’t improved over the past three decades, he says, “They’ve got numbers more like 60% for three-year survival.”
With grants from NCI and New York State, Brenner’s lab this year added a booster to its linac that will enable production of high-energy ions ranging in atomic number from helium to carbon. If the same long-range biological effects of carbon could be achieved with helium ions, he says, the size and expense of the accelerator required would be “inordinately” reduced. At 60 m in circumference and with tons of concrete needed for shielding, the synchrotron to be built by Mayo would be impossible to accommodate for hospitals in urban settings like Columbia’s.

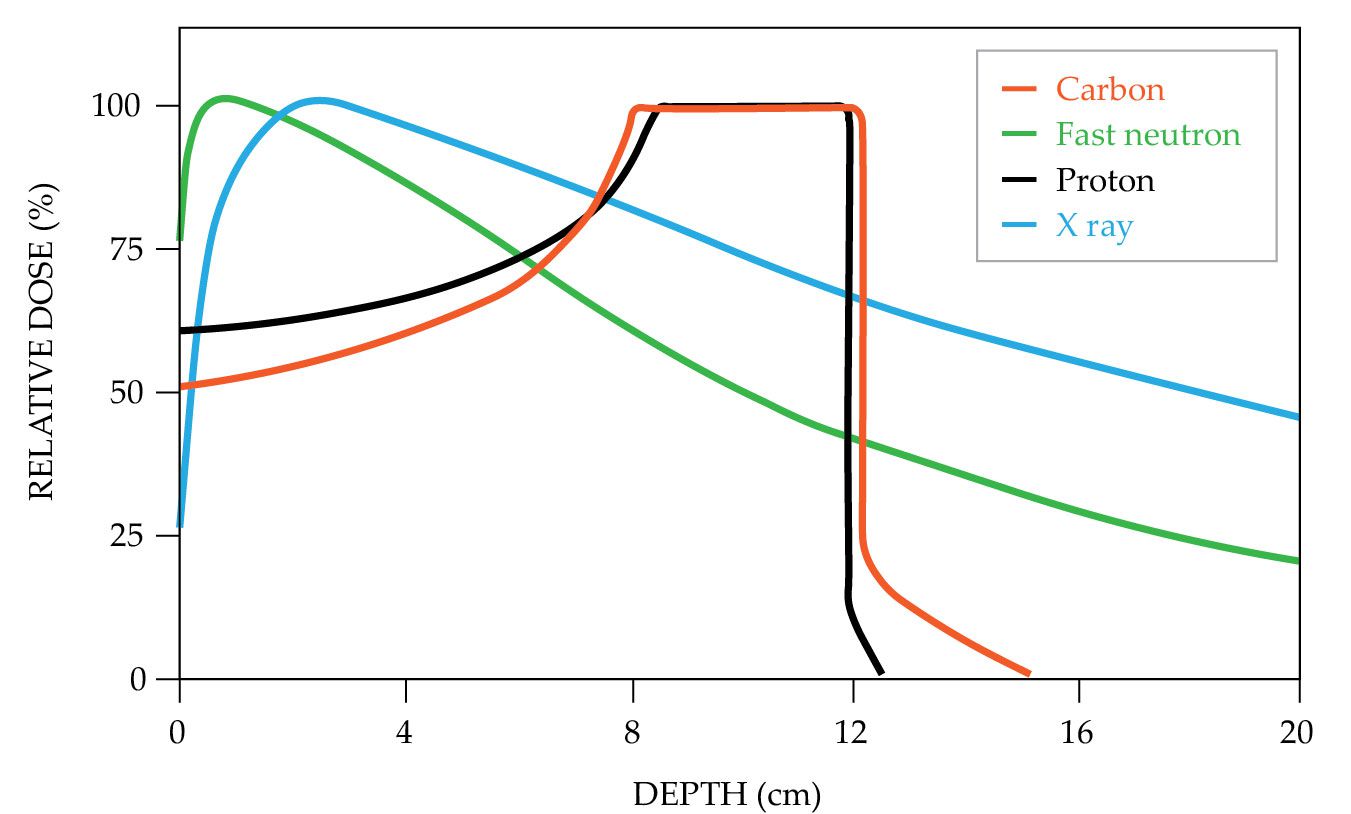
Charged-particle protons and carbon ions will deposit most of their energies at the target tumor site, leaving healthy tissue in front of and behind the lesion largely unscathed. X-ray beams begin to gradually lose energy soon after contacting the body. (Adapted from D. K. Ebner, T. Kamada, Front. Oncol. 6, 140, 2016, doi:10.3389/fonc.2016.00140
The Quantum Scalpel Project, which manages and operates Japan’s Chiba carbon-ion-treatment hospital, says it is developing a carbon-ion system that, at 20 m × 10 m, could be installed in an existing hospital.
Painting tumors
Unlike photons, both protons and carbon ions lose most of their energy all at once at the end point of their transit. Known as the Bragg peak, the phenomenon allows a beam to be precisely tailored to the shape and depth of the tumor, leaving the healthy tissue in front of and behind the tumor largely unscathed.
But carbon-ion therapy deposits more energy than protons, producing a greater biological effect. Carbon ions produce multiple irreparable double-strand breaks in DNA, while protons create only single-strand DNA breaks, for which cells have repair mechanisms. In addition, carbon beams scatter less—just 3 mm at 27 cm depth in the body, the maximum required to reach most tumors—compared with 13 mm for protons, says Lidestri. That makes for a sharper scalpel and a smaller “lateral penumbra” of damage to surrounding tissue. It also permits more precise beam scanning—so-called painting—to cover the entirety of the tumor mass.
Both protons and carbon ions can treat complexly shaped tumors such as those growing around the spinal cord, where a dose distribution that has a hole in the center can be created, says Jäkel. Carbon-ion beams can be more precisely shaped. Other cancers where carbon treatment is indicated in Germany include skull and brain tumors and a type of salivary-gland tumor.
In Japan, carbon-ion treatment is indicated for a long list of tumors. As of March, of the 14 000 patients that were treated with carbon ions at the Chiba center, prostate cancer was by far the most common, followed by bone and soft tissue, lung, head, neck, lacrimal, pancreatic, and liver cancers and postoperative recurrences of rectal cancers. Prostate cancer, for one, generally responds very well to conventional radiation therapy.
Lidestri notes that 50% of all current cancer patients will receive some form of radiation therapy, and about 15–20% of them are candidates for proton therapy, he says. About 12–13% of proton candidates might better benefit from carbon ions, he estimates. “I’m very careful to say that carbon-ion therapy isn’t a silver bullet. It’s just a different tool.”
One tantalizing implication from Japan’s positive results with pancreatic-cancer patients is an observed long-term reduction in metastasis. “The relatively long time from first diagnosis implies that carbon ions are doing something that’s improving the metastatic disease problem,” says Brenner. “In general, radiotherapy is aimed at the primary tumor, and the goal is to eradicate the tumor cells. If carbon ions are doing something good in two or three years, that tells us that something different is going on.”
Cancer grows because it can remain undetected by the immune system. In theory, the prevention of metastasis comes from the carbon-ion-induced double-strand breaks, which somehow create a new signaling path for the immune system to recognize cancer cells throughout the body, says Beltran.
But advanced cancer-treatment modalities other than carbon-ion therapy, including nonradiological ones, are also progressing. NCI has devoted “many millions” to support clinical trials comparing protons to photons, notes Buchsbaum, and it is currently funding four grants totaling between $20 million and $25 million over five years for studying helium- and carbon-ion beams in cells and animal models. NCI paid to have heavy-ion beams at Brookhaven and the Italian center qualified for those experiments. “NCI is supportive of carbon therapy; we’ve put a lot of money into the research,” Buchsbaum says.
Nonetheless, he says, carbon ions need to be evaluated in the context of all other treatment types. “The rest of the world hasn’t stood still. There’s [chimeric-antigen-receptor] T-cell therapy, immunotherapy, drug therapy, and better surgery. Carbon therapy isn’t competing in the same world as when Berkeley was doing experiments.”
More about the authors
David Kramer, dkramer@aip.org